
Interest and need for Wireless Body Area Networks (WBANs) have significantly increased recently. WBAN consists of miniaturized sensors designed to collect and transmit data through wireless network, enabling medical specialists to monitor patients during their normal daily life and providing real time opinions for medical diagnosis. Many wireless technologies have proved themselves in WBAN applications, while others are still under investigations. The choice of the technology to adopt may depend on the disease to monitor and the performance requirements, i.e. reliability, latency and data rate. In addition, the suitable sensor is essential when seeking to extract the data related to a medical measure. This paper aims at surveying the wireless technologies used in WBAN systems. In addition to a detailed survey on the existing technologies, the use of the emerging Low Power Wide Area Network (LPWAN) technologies, and the future 5G, B5G and 6G is investigated, where the suitability of these technologies to WBAN applications is studied from several perspectives. Furthermore, medical applications of WBAN are discussed by presenting their methodologies, the adopted wireless technologies and the used sensors. Given that each medical application requires the appropriate sensor to extract the data, we highlight a wide range of the sensors used in the market for medical systems. Recent and future challenges in WBAN systems are given related to the power consumption, the emergence of the Internet of Things (IoT) technologies in WBAN and others.

Avoid common mistakes on your manuscript.
Our world is facing a rapid growth of population accompanied with an increase in the average lifetime of individuals. According to a study presented by the World Health Organization (WHO), the population beyond 60 years of age would be around 2.1 billions by the year 2050 [1]. According to another WHO study, the rate of deaths in chronic diseases (such as diabetes, Parkinson’s, asthma, etc.) is increasing and will reach 66 \(\%\) in 2030 [2]. One of the reasons of this increasing is the late diagnosis of the patients. Early detection and effective monitoring would mitigate the impact of such diseases and decrease the healthcare cost. Besides the ageing population challenge, the modern lifestyle raises several health issues such as the inappropriate nourishment and the low physical activity leading to several expensive chronic diseases. Recently, the advances in wireless technologies ensure the remote monitoring of the patients. Many technologies have emerged the medical systems providing a continuous monitoring of the patients and helping the medical staff to diagnose and thus give medical directions. Being comfortable and not disturbing the daily activity, a network of sensors is installed in or on the patient body to extract some measures related to target diseases or health measures, forming the Wireless Body Area Network (WBAN). Communication between different parts to send data from the patient to the doctor and vice versa is done by several technologies [3, 4]. Due to the various available technologies, choosing the most appropriate technology, among the existing ones, is a challenging task [5]. Each of these technologies has its own functioning characteristics and should respect some constraints when used for healthcare applications. For that, the most common technologies are highlighted in this paper to study their suitability for WBAN medical applications. The WBAN technology usually consists of several small sensors and a centralized hub. According to the disease to monitor and the patient case, the sensors may have different roles, data rate requirement, power consumption and sizes. These sensors sample data and forward it using a wireless technique to the medical center via a power-rechargeable Personal Device (PD) having a greater computing capability relative to the sensors [6]. The continuous monitoring offered by the sensors allows the medical staff to update the patient’s condition. Hence, they may let the patients move freely as they are not kept in bed [7]. Moreover, WBAN permits patients to reduce their house or hospital stay thus reducing patients’ discomfort and reducing the risk of infection due to the long stay in hospitals [8, 9], especially in the case of an infectious pandemic like Covid-19 where the social distancing is needed for preventing the spread of the disease [10]. Also, WBAN may provide real time and secure collection and processing of medical data at the time where the hospitals were no longer able to receive more patients [11]. Thus, WBAN is one of the solutions that can reduces the one-to-one transmission of Covid-19 patients in order to stop the chain of this deadly pandemic [12].
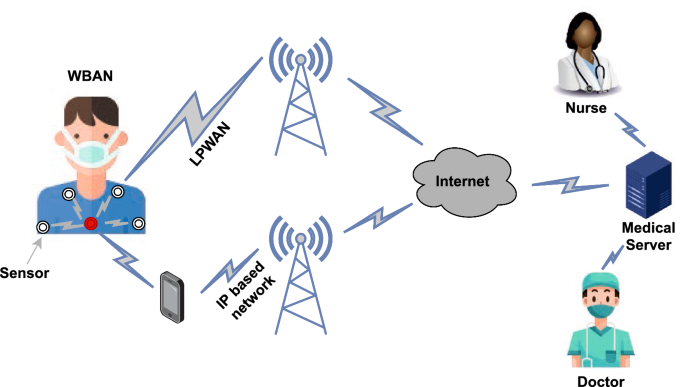
Sensors exist in a very large numbers on the market, in order to record physiological parameters during daily normal activity such as body temperature, heart rate, blood glucose rate and many other uses in several medical systems. Further, the requirements of these sensors, such as the needed data rate and the battery lifetime, may depend on the disease itself. This fact makes the choice of the suitable technology used to transfer the data from the patient body to the medical staff dependent on several parameters such as the reliability, the power consumption, the latency, weight, size, costs, etc. An overall pictorial representation of WBAN is presented in Fig. 1. The figure shows a remote medical monitoring system using WBAN networks, where multiple medical sensors are deployed on the patient’s body to measure multiple physiological parameters. The measured data will then be sent to the medical team over a network so that they can monitor the patient’s situation.
In Europe, in 2017 the healthcare expenditure is about 10 \(\%\) relative to GDP [13]. In USA, it is estimated that health care spending reached 3.81 trillion dollars in 2019 and would increase to 4.01 trillion dollars in 2020. It is projected that by 2028, health care spending in USA would reach 6.19 trillion dollars, where it is estimated that prices for medical services would grow at an average annual rate of 2.4 \(\%\) from 2019 to 2028 [14].
The insertion of WBAN in the medical applications generates great effects on the industrial and research world. Referring to a study published by Ericson, the revenue for ICT players will reach about 1307 billion dollars in 2026 with a rate of 11 \(\%\) for healthcare [15]. The spread of WBANs and the wide use of wireless technologies will benefit the economy and may reduce the medical bill.
Several surveys have detailed WBAN-related technologies and issues. Authors of [16] surveys the latest research of the coexistence of the wireless technologies and the interference mitigation in WBAN. The researchers in [17] discuss the latest developments in wireless technologies available for WBAN systems. The architecture, technologies, challenges and different aspects of WBAN are illustrated in [18], which describes the architectural limitations of the existing WBAN communication framework. In [19], the applications promoted by the WBAN system, fault tolerance, coexistence management and power consumption are discussed. Reference [20] discusses the WBAN communication types and present a comparison among some WBAN medical projects in terms of the used technologies. The work of [21] compares some low-power communication technologies based on the data rate, frequency band, security, topology, range and others, and focuses primarily on remote monitoring of old or chronically ill people. In [22], the paper focuses on the latest LPWAN wireless technologies that can be considered as the next-generation solution for WBAN healthcare monitoring. The main characteristics of WBAN systems with a list of the requirements of possible WBAN applications are also surveyed in [23], where the authors present the key issues of WBAN systems such as the energy consumption minimization problem, the coexistence of the wireless technologies and others. In [24], the authors survey the enabling wireless technologies for WBAN systems, the sensor devices, the application scenarios, and finally the interconnection of WBANs. In [25], the work delves into the ways in which the wireless technologies are transforming the IoT healthcare systems and outlines the future path for improving the Quality of Service using the new technologies. The authors of [26] investigate the functions of WBAN, its technologies, and a broader view on WBAN from the perspective of security and authentication. The reference [27] present a survey on the features of WBAN systems, especially communication, sensors, application requirements and security aspects. In [28], several types of miniaturized sensors used in WBAN are presented.
Despite the wide coverage offered by these surveys on the WBAN systems, several points are still not developed, such as the strong and the weak points of the classical and future wireless technologies (WiFi, Bluetooth, ZigBee, B5G, etc) and the IoT technologies (LoRa, Sigfox, etc) when used in medical applications. In addition, to date, there is no work summarizing academic research focused on widely spread diseases (such as diabetes, Parkinson’s disease, asthma and others), nor on the characteristics of the sensors used in the market to measure medical parameters for WBAN systems.
Then, the main contributions of this work are as follows:
The rest of this paper is organized as follows. An overview on WBAN systems and their characteristics and features is presented in Sect. 2. Then, a review of the main wireless technologies proposed for WBAN with a comparison between their merits and demerits is detailed in Sect. 3. In Sect. 4, a classification of some WBAN medical systems with their features, methodology and used technologies are presented. We provide some commercially sensors used in WBAN medical systems in Sect. 5. In Sect. 6, we present the main challenges with a discussion of open research problems. Finally, we conclude our work in the last section.
In this section, we present an overview on the architecture and the specifics of WBANs related to power consumption, latency, privacy, criticality of data and interference.
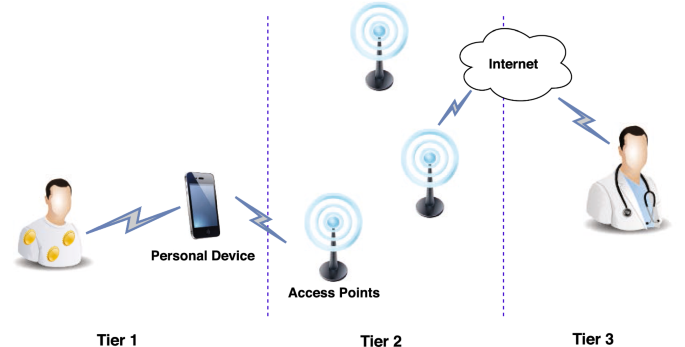
In WBANs, sensors are responsible for detecting physiological data, converting it into digital form and transmitting it to an access point. They can be placed on the human body (on-body sensors), near the body (wearable sensors), or implanted under the skin (in-body sensors). There are two types of sensors: the first type only measures data and sends it [29]. The second type called actuators, measure and send data as the first type and in addition, it can administer medication based on the collected data. The collected data are sent through wireless technologies to the medical server, where it can be analyzed and stored. This can be applied based on 2, 3 or 4 tiers depending on the architecture of the system and depending on the used technologies [20]. The most popular architecture proposed in the literature for WBANs consists of three tiers as shown in figure 2: intra-WBAN, inter-WBAN and beyond-WBAN [20].
Intra-WBAN refers first to the communication between the sensors and the PD, second between the sensors themselves [29]. Some existing schemes use cables to connect sensors directly with a PD, thereby avoiding the need for wireless network in the first tier [20]. In other schemes, data can be transmitted wirelessly to a coordinator or master node for further forwarding to the PD (multi-hop WBAN) or can be transmitted directly to the PD (single-hop WBAN) which forwards the data after processing to an Access Point (AP). The multi-hop and single-hop WBAN scenarios are described below:
Multi-hop WBAN: This kind of topology is adopted where the nodes range is short. Thus, to reach the PD, the message sent by a node may pass via the intermediate nodes.
Single-hop WBAN: in single-hop architecture, the PD receives the data directly from the nodes [20]. The power in single-hop configuration is higher than the one of multi-Hop but the delay is lower.
Inter-WBAN includes the communication between the PD and the AP using wireless technologies. Inter-WBAN tier connects WBANs with other networks that can be accessed by Internet. Inter-WBAN communication has two types of architecture: Infrastructure based architecture, which is used in most WBAN applications providing a more secure communication and Ad-hoc based architecture allowing for a quick and flexible disposition [30].
Beyond-WBAN refers to the communication between the AP and the remote medical center. A gateway is used as a bridge to perform the communication via Internet or cellular networks to transmit data to the medical staff. After receiving the data, medical specialists are allowed to analyse it to monitor the patient in order to provide necessary health advice [29]. This tier allows also to restore patient medical information which can be necessary to plan for an appropriate treatment [30].
Batteries of small size are used to power the sensors in WBAN systems. Some of these batteries, especially for the implanted sensors, are irreplaceable or must operate for multiple years without been recharged where replacing them may cause severe pain [29]. Therefore, the goal in WBAN is to obtain an efficient power system while using miniaturized batteries. The first point to consider to obtain an efficient power system is choosing a power efficient wireless technology for WBAN, which is discussed in the next section. Second, we have to let devices to go into sleep mode most of the time, in order to reduce the energy consumption. Third, minimizing the interference, since interference increases the energy consumption of a WBAN system where data should be transmitted more than one time [29].
Latency corresponds to the time taken by the data to travel from a device to another one[22]. It varies from values below one ms for 5G/6G to a few tens of milliseconds for 3G/4G, and can exceed one second for LPWAN technologies [31]. The low latency of data transmission ensures the successful transmission of real-time data to the medical center. The WBAN medical applications may be life critical if they cannot tolerate delays, especially in emergency situations, where delayed delivery of data may lead to patient death [22].
Privacy and security of the patient’s medical data are two indispensable requirements for WBANs. Privacy means that medical data, which is a highly sensitive form of personal data, must not be disclosed by people who do not have permission to use or view it, so that patients’ medical information is not abused. Security in WBANs refers to the protection of a patient’s medical data during collection, transmission and storage [22]. Any false data received by the medical staff may cause wrong treatments, and thus may lead to the patient death. As in traditional networks, WBANs have many security requirements [32], the main ones are as follows:
Availability: this requirement aims to ensure that the patient’s data can be accessed by the medical staff anytime it is required. Especially for life-saving data which may result in loss of life in case of non-availability of data [30].
Confidentiality: corresponds to the protection of medical data from disclosure. Data eavesdropping breaches privacy which may cause a fatal damage towards the patient. Encryption of medical data over a secure channel provides the confidentiality of data [33].
Authentication: allows to verify that the data is sent by a trusted end device. End devices in WBAN compute a Message Authentication Code (MAC) for the data by sharing a secret key which makes the coordinator realize that the data is received from a trusted end device [34].
Integrity: this requirement aims ensure that the received data has not been manipulated by an adversary using data authentication protocols [33].
Despite the tremendous research work during the last decade, Privacy and Security for WBAN is still a hot topic to study. Many cryptography techniques and algorithms are proposed in several works in the literature to achieve secure WBAN systems. Hereinafter, we list some of the last concerned studies. Authors of [35] propose a strategy of random key deployment scheme. Data in this scheme is transmitted from node to node (through an ad-hoc wireless network) which resists the attack of a cracker. The work of [36] proposes a secure protocol for WBANs where a group of nodes creates trust by forming an authenticated group to associate correctly to the intended patient. In [37], the authors present a physiological-signal-based key agreement (PSKA), which is a secure scheme for communication within a WBAN. PSKA allows neighbouring sensors in a WBAN to agree on a shared cryptographic key in an authenticated manner and without any need of initialization or setup, using the obtained physiological signals. Dynamic password-based authentication scheme is proposed in [38]. The system uses a custom password computation algorithm in order to make the password for each login dynamic and confidential. In [39], the authors propose a lightweight scheme for WBAN authentication based on two secure protocols, the first for authentication and the second for re-authentication in order to protect the sensors anonymity based on the hash function. The proposed authentication cryptosystem for WBANs in [40] is based on an algorithm using a combination of an elliptical curve cryptography with bi-linear pairing schemes. The proposed study in [41] uses firstly the KBS (Key Generation Procedure) keys and Hash algorithm to improve the WBAN’s security. Second, KAISC (Key Generation Algorithm for Inter Sensor Communication) is used for inter WBAN communication. The authors in [42] design a secure key agreement protocol and anonymous authentication for WBAN using XOR and simple hash operations. In [43], the work explores the use of biometric characteristics to provide a secure data communication in a WBAN.
In some medical WBAN applications, the data is critical and cannot tolerate a long response time [44]. Hence, real-time transmission is required with guaranteed performance. Sensors in real-time WBAN applications should instantaneously sense and transmit feedback to the medical staff to process the obtained information while achieving a bounded delay latency. With recent advances of WBAN systems, real-time applications have attracted prominent attention from researchers. The work of [45] investigates real time sensors to diagnose the cardiac patients. Also in [46], a WBAN system for electroencephalogram real time monitoring is proposed, where physicians can monitor real time signals via Internet. Another real time WBAN application is proposed in [47] where electrocardiogram measurements are sent to a smartphone in real time.
In real time WBAN applications, sensors may differ in their criticality while transmitting their data [48], where the degree of criticality for each sensor depends on its emergency level and on the nature of the measured data [23]. Distinguishing the criticality of sensors is an important issue to assign a specific priority level to each sensor in WBANs. This distinction between non critical and critical data and, therefore, between high priority and low priority allows data to be scheduled in order to minimize collisions. Moreover, the same sensor may be in different critical states [19]. If the data gathered by a sensor exceeds the value of normal threshold, this indicates that the data has a high critical level and it should be transmitted with high priority. Minimum delay and high reliability level are two prerequisites for data of high criticality, e.g. the data sent by an application for monitoring of elderly heart patients. Moreover, by determining the level of criticality, doctors can examine patients according to their level criticality, which enhances the physician time efficiency [49].
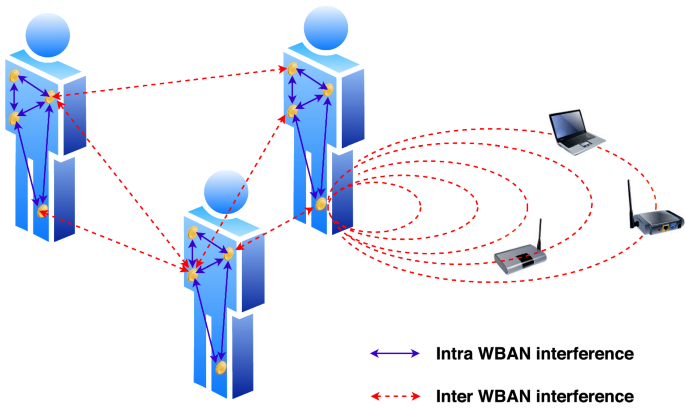
The ever growing of WBANs results in increasing the interference, which is a real challenge [50]. The interference can affect the performance of networks and may also affect the power consumption of the sensors as a result of the frequent re-transmission when the interference prevents the data to arrive correctly to its destination [50]. As shown in Fig. 3, the interference in WBAN systems can divided into two kinds. First, intra-network interference, as a result of the asynchronous transmissions between near sensors. Second, the inter-network interference, where external sources operating at the same frequency bands of WBAN cause interference [51]. Inter-network interference may also occur when the data of two or more WBANs is sent simultaneously. To ensure the quality of the signal in WBAN, it is necessary to avoid or mitigate these two forms of interference [52]. Authors in [53] and [50] shows that the increase in the number of WBANs and the increase in the data rate have a negative impact on the packet delivery ratio. The effect of distance, orientation of transmitters and receivers, packet size, and the transmission power level on the interference level between the sensors in terms of the packet loss rate was presented in [16] and [54]. In the following, the techniques adopted to mitigate the interference in WBAN systems are presented.
Time Division Multiple Access (TDMA) is a technology that allows a number of nodes to share the same frequency channel by adopting a time slot allocation for one node transmission. TDMA solutions are more suitable for intra-WBAN interference rather than inter-WBAN interference mitigation [16]. Moreover, the main problem in TDMA is the delay in critical medical data delivery that may exist when the time frame is divided into time slots less than the number of nodes [55].
In Frequency Division Multiple Access (FDMA), each channel can carry digital data at the same time without interfering with other channels. The limited number of available channels is the main problem in FDMA [16].
Code Division Multiple Access (CDMA) is a multiple access technology, where the users are provided with codes, which are orthogonal to each other. This means that all users can use the same frequency and transmit at the same time [56]. CDMA is very effective for multi-sensors transmission scenario in WBANs.
With the emerging of new wireless technologies such as 5G and B5G, several multiple access techniques such as Non-Orthogonal Multiple Access (NOMA) and Sparse Code Multiple Access (SCMA) seem to be promising to alleviate the interference issue [57]. NOMA allows allocating one frequency channel to multiple users at the same time within the same cell, offering a high throughput and low latency [57]. SCMA allows non-orthogonal transmissions of multiple users on the same resource blocks with different codebooks. With sparse codebooks, SCMA reduces the collision between users[58].
Choosing the priority of a sensor can also mitigate the interference. The data collected by each sensor in a WBAN differs in their delay requirements, for example the emergency medical data require minimum delay, so it has the higher privilege to access the channel. Beside the priority of the sensor, it is necessary to classify the WBAN priority among inter-WBAN in multi-WBANs coexistence scenario [59]. To select the critical data among multiple sensors in multi WBANs coexistence scenario, researchers define the health critical index [52] where it considers the sensor priority and the WBAN priority. In [60] an algorithm is proposed where the sensors in multi-WBANs coexistence scenario are sorted from large to small value of the health critical index to select the more critical sensor.
The use of wireless technologies for the exchange of information collected by the sensors, eliminates the needs of cables between the sensor and the access point. The choice of the appropriate wireless technology is an important part of the WBAN systems where an inappropriate technology can result in waste of time and energy. In this section we present the characteristics of the main proposed technologies for WBAN.
Bluetooth was designed for short range wireless communication, where a number of Bluetooth devices form a short-range personal network known as a piconet [44].A single piconet includes a device which acts as a master and controls up to seven devices known as slaves. A slave device can only communicate with a master device, but cannot directly communicate with other slave devices. Bluetooth devices operate in the 2.4 GHz ISM band with a coverage range from 1 to 100 m. The maximum data rate is 3 Mbps and the time needed for connection setup and data transfer is about 100 ms [44]. For WBAN systems, Bluetooth can be usually used for the communication between the sensors and the PD in the first tier, it is free and supported by most devices. It can be used for sensors of relatively high data rate requirement, but it is not an ideal choice in terms of power consumption.
Bluetooth Low Energy (BLE) was designed to wirelessly connect small and low-power devices to mobile terminals. BLE network topology is a star. BLE device can be a part of multiple piconets and can operate both as a master or slave device. Thus, these devices can play multiple roles at the same time which enables the communication between piconets 61, 62]. BLE offers a data rate up to 1 Mbps [24, which makes it a suitable choice for WBAN applications. Moreover, thanks to the low duty cycle, BLE consumes 90 \(\%\) lesser than the power required by Bluetooth. This leads to extend the lifetime of the sensor’s battery in WBAN systems. But BLE has a range of 10 m, which make it difficult to be used in other than the first tier in WBAN. Synchronization can be done in a few milliseconds compared to Bluetooth seconds which is very valuable for latency-critical devices used in WBAN health-monitoring applications. It uses 2.4 GHz frequency and the time needed for connection setup and data transfer is less than 3ms [21, 44].
ZigBee is a wireless technology providing a long battery lifetime, a low data rate and a secure networking as explained below [63]. ZigBee is an easy network to install and configure, it supports various network topologies and a large number of nodes. Its equipment can operate for a few years before the battery needs to be replaced which make it one of the technologies used in many medical applications in WBAN. ZigBee is a secure networking where it offers three levels of security mode to prevent the data from being changed or accessed by attackers [64]. With a range of 100 m, ZigBee operates at 2.4 GHz, 915 MHz and 868 MHz frequency bands with a data rate of 250 Kbps, 40 Kbps and 20 Kbps for each of the operating frequencies respectively. For WBAN, ZigBee targets medical applications that require frequent measurements and text-based data transmission with low power consumption. It can be used for the body temperature monitoring, for the pulse monitoring and others [64]. Due to its low data rate, ZigBee is insignificant for some WBAN medical applications which requires high data rate and it is difficult to implement it in hospitals for multiple patients [65]. Thus, another significant disadvantage of ZigBee for WBAN applications is due to interference in 2.4 GHz band where many wireless systems operate.
WiFi provides reliable, secure and fast communication. It is integrated in all smartphones, tablets and laptops. WiFi comes generally with four standards (802.11 a/b/g/n), it can operate in the 2.4 and 5 GHz bands and has a coverage of 100 m [66]. It is able to deliver data rates of up to 600 Mbps [44]. It is ideally suitable for large amount of data transfers with high-speed wireless connectivity that allows voice calls and video streaming. In WBAN systems, the use of WiFi is not preferred in the first tier due to its high power consumption [65], it is used for the communication between the PD and the APs in the second tier in some WBAN medical applications. As Bluetooth and ZigBee, WiFi occupy the ISM bands, where serious co-channel interference may occur.
The wide usage of the wireless spectrum has many drawbacks such as the interference and the absorption of radio frequency radiations [67]. One of the revolutionary solutions to overcome these issues is Light Fidelity (Li-Fi) for indoor usage and for high speed data network [68]. Li-Fi networks support the transmission of data through illumination of Light Emitting Diode (LED) bulb. It provides a high data rate up to 1 Gbps or even more with a low cost and low power consumption thanks to the use of LED illumination. From the medical perspectives, LED may be available in the homes and hospitals, which makes the Li-Fi applicable for WBAN medical applications. Furthermore, Li-Fi provides high secure and private connection, low interference and high bandwidths [69]. This helps to protect the privacy of the patient while ensuring a reliable communication. By contrast, the limitation of the use of Li-Fi is due the need to light source. This drawback prevents the cross-walls communications and imposed the communication to be short range [69].
Low Power Wide Area Networks (LPWAN) technologies become very popular in industrial and research communities thanks to their long range and energy-efficient communication. Due to efficient adopted protocols, the lifetime of the end-nodes of the LPWAN-based technologies is of order of years instead of days or months [70]. Hereinafter, we show the main characteristics of five popular LPWAN technologies: LoRa, SigFox, INGENU RPMA, NB-IoT and WiFi HaLow.
The LoRa (Long Range) Alliance proprietary LPWAN technology consists of two main components, LoRa and LoRaWAN protocol. LoRa is a physical layer modulation scheme used in LPWAN technologies that drawn several research for healthcare systems due to its low cost, long coverage area, and long lifetime of the sensor [71]. LoRa modulation uses orthogonal Spreading Factors (SF) [72]. This enables multiple packets of different SF to be in the same channel concurrently without interference [71]. The number of data bits modulated depends on the used SF, higher SF implies that there are fewer data to encode per second, compared to lower SF. Sending the same amount of data with higher SF needs more transmission time.
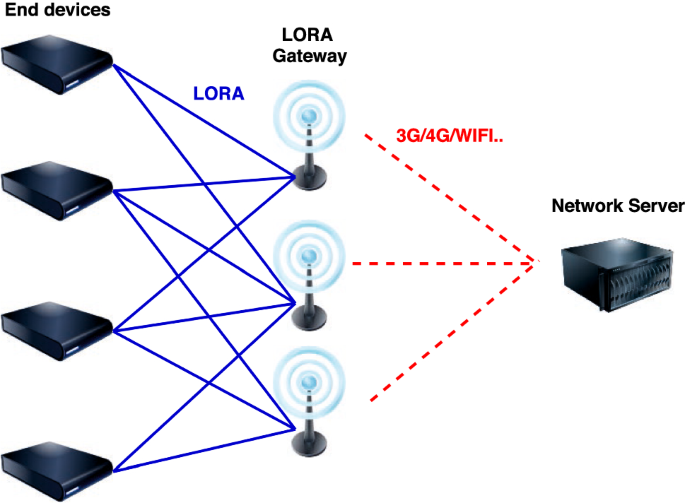
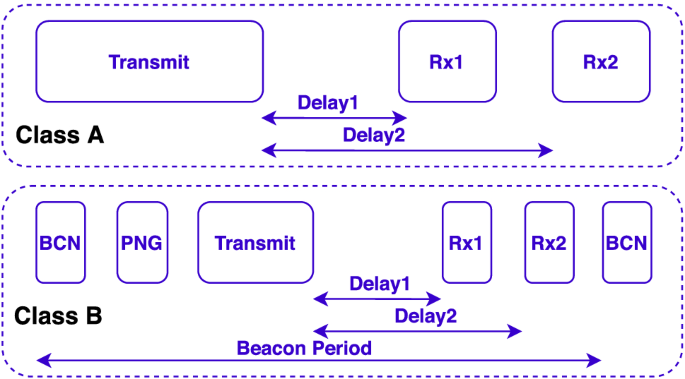
In turn, LoRaWAN protocol is a wireless communication protocol developed by LoRa Alliance. The architecture of a LoRaWAN network supports a two-tier topology (see Fig. 4), and it is based on three different types of devices: end-devices, gateway and network server. Such architecture is helpful for WBAN because end-devices collect information and sends them to gateways directly by combining the two tiers 1 and 2 and subsequently eliminating the use of a PD. Then, the data is transmitted from the gateways to the network servers using any types of IP infrastructure such as 4G or WiFi as shown in Fig. 4 [73].
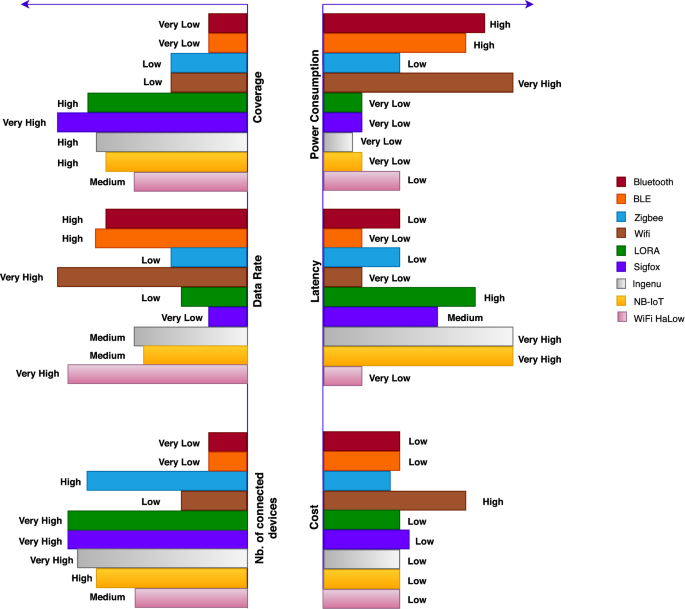
As a conclusion, we can say that the choice of a technology depends on the requirement of the sensors, and the requirements of the system and its capability to provide energy. For example, for sensors of very high data rate requirement we can use WiFi. For sensors that need to transmit continuously, LoRa becomes an unsuitable choice but it is an ideal choice to monitor patients that circulates over a large area and uses sensors of low data rate that requires low power consumption. The table and the diagram presented below help us choose the suitable technology for any medical system according to its needs and requirements.
With the ever growing of the wireless communication-based applications, new cellular technologies have been proposed in order to tackle the challenges of the high data rate, the massive number of connected devices, the low latency and others. In this section, we focus on the cellular future technologies and their impacts and challenges related to the WBAN applications.
The fifth-generation (5G) of cellular network technology is expected to provide a very high data rate up to 10 Gbps, low latency close to the millisecond, high reliability, wide bandwidth of more than 100 MHz, high capacity, interference mitigation, massive number of connected devices and secure network [91].
In WBANs, 5G could generate significant improvements for medical applications, especially for urgent and critical applications requiring a real time transmission of data and high data rate. 5G can achieve a very high improvement for tele-surgery using robotic platforms with audio, video and haptic feedback [92]. It is also an efficient solution for the accurate real time continuous monitoring of patients, and for detecting the position of the patient in case of abnormal situations and it can be used for speedy transmission of medical images and videos [93]. However, power consumption of 5G remains an important issue in WBAN, especially for miniaturized sensors that need to operate for multiple years [94]. For beyond fifth generation (B5G) mobile communications, it should achieve a system of capacity more than 100 times compared to 5G networks, high data rate in the range of terabits per second, low latency, high reliability which can be very promising for healthcare applications in WBAN [95].
6G will use the terahertz signal for transmission which increases the bandwidth and the data rate. The requirements of 6G communication technology for future healthcare are high data rate (more than 1 Tbps), low latency (less than 1 ms), high reliability, high mobility support (more than 1000 km/h) and high bandwidth (three times higher than 5G) [96].
5G and B5G provides 2D communication, whereas 6G will shift to the 3D services using holographic communication which will revolutionize the intelligent healthcare systems especially for tele-surgery which requires a very high data rate. Other applications such as remote patient diagnostic and medical treatment supervising will be also feasible, where doctors can diagnose remotely using holographic communication which can relieve the economical and physical burden for the patients [97].
WBAN supports many applications and has great practicality and advantages in daily life where it provides the advantages of freedom of movement, security, low power consumption, real-time data delivery and low cost. In addition to the main WBANs application in the healthcare field, to monitor patients efficiently, WBAN applications can be also used in entertainment, military, public security , sports and other fields [19]. The classification of WBAN applications is as follows: non-medical wearable applications and medical applications which can be wearable or implanted. In military and public safety, WBAN applications are used to improve the soldiers’ performance in military situations. In this case, it is important to monitor the soldiers’ vital signs and stress levels [98]. Moreover, in sports monitoring applications, the athletes physiological data collected during a game such as temperature, heart rate and body position may avoid critical situations [99]. As well patients who have recovered from an accident, can remotely perform exercises with the supervision of the medical staff [100]. For medical systems, [101] resumes the main sensors used for WBAN systems in order to monitor the development of various diseases such that diabetes, asthma, Parkinson and others. The biosensor gyroscope and the glucometer are used for diabetes monitoring. For cardiovascular disease we can use pulse oximeter, heart rate sensor and ECG sensor. Allergic sensors are used for asthma. For Parkinson disease we use motion sensors and Accelerometer. These sensors need to send their data using wireless technologies to an external medical server where it can be analyzed and stored. This can be applied based on 2, 3 or 4 tiers (see Fig. 2) depending on the architecture of the system. In order to develop a reliable and energy-saving system architecture, WBAN-based applications must overcome many difficulties, such as the battery capacity of the sensor, cost, security and others. Many research have conducted in this regards, hereafter we present many works concerning some WBAN medical applications for treatment and monitoring, where we focus on the methodology of each system, on the used technologies and the used sensors. We present some systems for diabetes patients, body temperature monitoring, asthma monitoring, Parkinson’s disease, depression monitoring, Electrocardiogram ECG, oxygen saturation monitoring and finally, we present a case study about Covid-19.
The proposed WBAN in [76] consists of 3 tiers, for the first one, the LifeScan’s OneTouch Ultra glucometer (invasive sensor) or the Combo glucometer (non-invasive sensor) are used to measure the glucose blood level, then the collected data is transferred using ZigBee or Bluetooth to a smartphone which acts as a gateway to transmit data to the AP using the IEEE 802.11, the WiFi or the GPRS communication medium. In [77], doctors can monitor remotely the patient’s glucose level using an implemented glucometer sensor. ZigBee is used to send the data wirelessly from the sensor to the application system. The proposed WBAN in [6] consists of 3 tiers. The home of a monitored patient is covered using a ZigBee network, the data is collected and processed then transmitted to the cloud service.
The sensor NTC Thermistor in [102] forward data to the PD wirelessly through ZigBee, The PD collects, processes and uploads the data through GPRS. The proposed WBAN in [103] consists of 3 tiers, where one Raspberry Pi device connect many patients and uses Bluetooth to continuously receives the messages from the sensor, then the Raspberry Pi transmit the data through cables to the main server. In [104], the sensor DS18B20 is used to monitor the temperature. The authors use an Arduino microcontroller to build a healthcare portable monitoring system. The system is equipped with an SD card, a screen, and a 2.4GHz WiFi module to transmit data to the server. The LM35 temperature sensor in [105] send the collected data to a microcontroller via ZigBee wireless technology then the system sends its real-time data through wireless local area network to a medical monitoring database. Data collected from sensors in [106] are sent to a LoRa gateway through a LoRaWAN network, the gateway forwards the data via 3G/4G links to a server.
The system in [107] is designed using ZigBee wireless technology. The data is collected by an IR sensor the processed using an Arduino micro-controller which uses XBee network to transmit the data to a remote computer. The data collected by the sensors in [108] is processed by a microcontroller, then sent via WiFi to a main location. For efficient monitoring, a message is sent to the medical specialists in case where the collected data sent to the microcontroller is abnormal. The sensor Polar belt in [109] transmit the data to a PD through ZigBee or Bluetooth. The PD provides the user with graphical and audio interface and uses WiFi or mobile networks to transfer health data to the medical server. In [110] the patient is monitored by the heartbeat sensor TCRT1000 which is interfaced with Arduino mega microcontroller. For an effective monitoring, a message is sent via GSM to the doctor in case where the measured value exceeds the normal range.
The system in [111] consists of 3 layers as follows: the sensor layer, the personal network layer and and global network layer. The location of the user is monitored by the ”Qstarz BT-Q1000P” GPS, the Physical activity by a tri-axial motion sensor and the Air pollution is monitored by the airborne Aerocet 531 Particle Counter. The base station is formed form a Nokia-N810 tablet, which is connected to the motion sensor wirelessly via IEEE 802.15.4, to the GPS receiver via Bluetooth, and wired to an airborne particle monitor via a serial USB cable. In [112], Bluetooth is used to send data from the sensor to the smartphone, the transmission of data is only done when a wheeze is detected. In [113], the collected data is transmitted from a digital bracelet and from an acoustic sensor through a LoRaWAN network. The digital bracelet is used to detect the presence of nitrite while the acoustic sensor is used to detect the wheezing sound from the chest of the patient.
In [114], data transfer from the actigraphs sensors (versatile and affordable sensors) and the hub is performed using IEEE-802.15.6 standard. The system in [115] uses a number of miniature wearable wireless sensors (based on SHIMMER platform) to monitor patients with severe movement fluctuations. Gateways such as smartphones are used to send data over the Internet. The system of [116] consists from a wearable smartwatch to measure the movement of a patient and to send the data to a database server through a handheld (Smartphone). The handheld communicates via Bluetooth or WiFi with the smartwatch while the communication between the handheld and the server is done through HTTP requests.
An application was designed in [117] using an Android platform, the application is installed on a smartphone to notifies the caregiver in case of any abnormal situation by generating an alarm. The sensors used are the accelerometers and the barometric pressure sensors.
The system in [118] uses ZigBee wireless technology for signal transferring. The system consists of two mobile platforms, the first for signal acquisition while the second for monitoring based on the analysis of the ECG signal. In [119], a WBAN ECG remote monitoring system is presented where a power management strategy in proposed to improve system lifetime. An algorithm is also proposed in the study to classify ECG signals as stable or not. The paper [120] presents an approach for WBANs based ECG monitoring systems to identify the critical and non-critical signals using machine learning and to minimize the miss-classification of critical data.
In [121], Near InfraRed Spectroscopy (NIRS) is used to measure the blood oxygen saturation, then the data is sent to the doctor form the PD through GPRS/WiFi/ZigBee networks. In [122], a finger pulse oximeter is used to read the SpO2. The signal processing unit receive the readings via Bluetooth to take a decision to send an alarming SMS or not. The system in [123] consists of several sensors including the ”My signals SPO2 sensor” oxygen saturation sensor, where data is sent to a PD by using a LoRaWAN network.
Data rate requirements of the sensors for medical systems varies from less than 1 kbps to more than hundreds of kbps, this refers to the nature of the data to be sent, for example the heartbeat should be reported continuously whereas the temperature should be sent once in a while. For diabetes patient the data rate required is a few of kbps, for body temperature we require a very low data rate (less than 1 kbps), a hundred of kbps are required for the monitoring and treatment of asthma and Parkinson’s patients and for the monitoring of the heart rate. Also, the Electrocardiogram ECG requires a hundred of kbps while the data rate required for the oxygen saturation monitoring is a few kbps. The power consumption highly depends on the data rate and on the used wireless technology where the choice of the wireless technology for each tier is one of the mostly important factors in WBAN systems which depends on the requirement of each system is terms of the needs of data rate, needs of coverage, the needed level of security and others. For the cost, most of the medical applications mentioned above are of low cost where this is one of the most important characteristics of WBANs. On the other hand, we have noticed the use of the smartphone in the majority of research, especially those of 3 tiers. Smartphones can collect analyze, and display the data via mobile applications. The use of smartphones reduces the cost of healthcare systems where many applications (such as cameras and accelerometers) are free [21]. However, smartphones are not effective for visually impaired patients or elderly people who cannot use the technology.
In this section, we investigate the WBAN application for Covid-19 case study. Monitoring Covid-19 remotely may highly reduce the healthcare cost and increases the hospitals’ capacity by decreasing the physical presence of the patients. The needed data to collect, the required technology and the system’s basic requirements will be discussed in this subsection. To monitor the symptoms, biomedical parameters like temperature, heartbeat, respiration rate and oxygen saturation must be collected, analysed and sent to the medical staff [124, 125]. Such WBAN systems face a major challenge in balancing between acquisition of high fidelity data and minimizing network energy consumption and data latency while achieving a fast real time interaction in urgent case. By using biomedical sensors for health monitoring with the wireless technologies, it is possible to send medical reports to the medical staff where doctor’s advice is obtained without the need of any physical movement. This WBAN system comes as a rescuer for Covid patients who need to be under monitoring, especially for elderly patients and for patients suffering from chronic diseases. Hence, two scenarios are proposed for transmitting the patient’s data to the medical server. In a first scenario, for the first tier it is possible to connect the sensors to the PD using BLE or ZigBee providing a data transmission for short distance which is convenient for the WBAN’s first tier. After been processed, the data must be sent to a gateway using WiFi or cellular networks. Finally, the data is received by the medical staff where the patient is diagnosed and an advice should be given in case of unstable condition. In another scenario, data is sent directly from the sensors to a gateway through one of the LPWAN technologies providing a long range, low data rate and high network lifetime which are convenient for our case. Latency remains an issue to concern, where the reception of the physiological information by the medical server at the required time is a condition for the success of the remote medical monitoring system. It is worth noting that data can be compromised by an attacker. Hence, security protocols are required in the system to protect the sensitive medical data and to maintain the patients’ privacy.
In the previous section, we have listed some WBAN systems for medical applications including the used sensors in each system. Choosing the sensor is an important part in WBANs in terms of its role, its power consumption need, its size and its lifetime. A large range of commercially sensors is used in order to measure the physiological parameters for WBAN systems. The aim of this section is to present some of many sensors found on the market for glucose monitoring, temperature monitoring, asthma monitoring, monitoring of heart rate, accelerometers and gyroscopes, and monitoring of blood pressure. Table 3 represent the position, the work technique and a classification of the data rate requirement for each one of the sensors.
The accelerometers/gyroscopes are used for monitoring of physical movement. Glucometers are used to measure the amount of glucose in the blood. Recently, this can be done through the infrared technology and the optical sensing. Temperature sensors are used to measure the temperature of the body and some of them can send signals in case of an abnormal situations. Heart rate sensors measure the amount of beats per minute. They are used to monitor the heart rate of a patient in order to diagnose heart diseases. Blood pressure sensors are used to diagnose and monitor high blood pressure which is a common risk factor for heart attacks and strokes. The important features to consider in choosing the WBAN sensors are power consumption, the size, the weight, the cost and the accuracy. It is important to achieve balance between these features because some of them are conflicting. For example, the more power a system demands, the largest the volume of its battery must be, while the need in WBAN medical systems is for a low power system with a battery of a small volume.
Table 3 Some market sensorsThe major requirements for WBANs are to achieve a secure and private network with high degree of reliability. Additional requirements such as low latency, high power efficiency and less absorption of radiations by the human body are also of high importance. This section details the most pressing challenges and some research directions to overcome them.
Power consumption still one of the major issues where long lifetime of sensors is required, especially for implanted sensors that may need to operate for several years with a disability to replace their batteries. Many research was prompted by this fact to study the ways of energy savings by maximizing the sensors’ sleep time and by avoiding collision and thus avoiding the retransmission of data. Several researchers have studied techniques for recharging the battery based on body movement. Other researchers have designed a wireless self-powered sensor which is powered by the human body [152], while in [153] researchers have studied the short-range wireless transmission of energy to electronic devices.
Also in [154], a research work proposes the schedule-based charging algorithm which uses wireless power transmission technology to charge the implanted sensors in WBAN. Further, with the transition to 5G, the optimization of power efficiency is still being investigated. Thus, more research on 5G based WBAN are still needed to achieve high power efficiency required by these networks. Here, Link adaptation and duty cycle may play an essential role [94, 155].
The absorption of radio-frequency radiation may have negative impact on the human body, specially for sensitive organs. For instance, the eyes exposure to an infrared radiation is a high concern where the exposure to radiations of rate of absorption per unit weight of 8W/Kg in the head or chest for a time of 15 minutes can leads to the risk of tissue damage [156] knowing that the maximum permitted exposure rate value, is 2W/kg in Europe and 1.6W/kg in the USA. So, one of the principal challenges in WBAN is to reduce the radiations rate [157]. To minimize the energy absorbed by the human body, the sensors must maintain their power efficiency to maintain a low-power absorption [158]. Thus, WBAN equipment should be able to run less time and use low power transmission. This is related to the choice of technology and the methodology of the system where LPWAN technologies can become one of the solutions due to their low transmission power and low duty cycles.
As mentioned in section 2.2.3, several security prototypes for WBANs have been described in the literature. Despite these studies, security and privacy of medical data in WBANs remains two huge challenges requiring appropriate mechanisms where currently, much research is going, and several open issues exist such as:
First, in the near future, WBAN will become more pervasive, where the patient data will be shared with family members, doctors, hospitals, pharmacies and others which requires a high level of consistent policy sets to protect the patient’s privacy.
Second, WBANs may be vulnerable to various attacks, the authors of [159] classified these security attacks into two kind of attacks: external and misbehaviour. For the external attack, it can be easily handled by traditional security mechanisms while it cannot handle the misbehaviour attacks which require more research studies.
Third, another area that needs attention is the area of trust management. Trust is the degree to which a node can be considered trustworthy, reliable and safe when interacting with other nodes. A survey about latest research about trust management for WBAN is presented in [160].
Fourth, complex security mechanisms for WBANs require more power resources, so a balance between many factors such as security, power consumption, efficiency and practicality is very crucial and need more researches to achieve the widespread use of the medical applications in WBANs.
Some recent analysis about security and privacy issues are presented hereinafter. In [161], the paper details the security and privacy issues and challenges raised by the increasing use of the IoT. Then, the authors analyze existing solutions that address these challenges, and they suggest new solutions to address the existing ones. Also in [162], the study provides an IoT security analysis, where it examines the potential threats and identifies the countermeasures and their limitations paying an attention to the mechanisms of security of the IoT protocol. The work of [163] outlines and discusses the general attacks that can plague the IoT devices and networks. It then evaluates LoRaWAN’s security mechanisms, and whether that security can be effectively compromised. The paper [164] studies the possible threats within pacemakers. The paper attempts to show if it is possible to hack a current model of an industrial pacemaker.
LPWAN are promising technologies due to their low power consumption and their long range, but it remains some modification to do in the LPWAN protocols in order to support e-health applications. Urgent and On-demand transmissions are highly requested in the medical applications, but are not supported in many LPWAN protocols, such as LoRaWAN, where the protocol is mainly designed for Uplink transmissions. Other challenges related to the mobility of the patients have to be addressed by these protocols since many of them do not support the mobile things communication [165].
Transmission reliability is a critical issue ensuring the performance of a WBAN [101] where the monitored data must be received correctly by the medical staff or it can be fatal if a life-threatening event is not detected. Reliability includes the delivery of data in a reasonable time, and a guaranteed delivery of data. The unreliability has main causes as: low transmission range, interference, inefficient routing and others [166].
Quality of service (QoS) is one of the basic characteristics to achieve a reliable network. Reliable QoS indicates the arrive of the packets on correct order and on time [19]. According to [167], QoS is a key part of the medical information transmission in WBAN, where critical applications require the highest QoS. High QoS requires a high throughput which is an important part to improve the system performance. The throughput is proportional to the packet payload and inversely proportional to the transmission delay. QoS also requires a minimum delay in order to ensure the data effectiveness. Another requirement is to maximize the network lifetime by controlling the main sources of energy lost [48]. 5G may be a good candidate in helping WBAN system to achieve high QoS since this generation will ensure high data rate, high reliability and very low latency. However, this may increase the energy consumption. Therefore, we have to compromise between these factors to achieve a good performance.
Interference in WBANs is one of the major open issues which essentially needs to be addressed. The requirement to support many different sensors on the human body in WBAN, in addition to the coexistence of many WBANs within the same area, makes the coordination between the WBAN systems necessary and challenging [168]. The problem of interference can also arise between WBANs and the other wireless networks in the ISM bands leading to a low health data reliability, energy inefficiency and high latency caused by the signal distortion.
Recently, several methods have been proposed in the literature to mitigate interference in WBANs. Hereinafter, some of these published studies. In [169], a scheme based upon Efficient Mitigating Rules ”EMR” is proposed at the level of the central coordinator to mitigate interference. The work of [170] formulates the channel selection of the coexisting coordinators in WBAN. Two algorithms are proposed to achieve the Nash Equilibrium of the formulated game. Paper [171] considers node-level interference mitigation instead of treating each WBAN as a whole. The main objective of [172] is the scheduling of the nodes in the WBAN in an interference free manner. Authors proposes a priority-based scheduling algorithm where the nodes priority is taken into consideration for scheduling the body sensors. The work of [173] proposes a scheduling technique to mitigate interference under a machine-to-machine based medical WBAN. In the work of [174], a distributed TDMA scheme is proposed to minimize the probability of collision between nodes in coexisting WBANs. Furthermore, it is well-known that power control is used to mitigate interference, where many studies prove its efficiency in reducing interference. In order to mitigate the inter-WBANs interference, [175] proposes a power control game-based approach which is based on the patients’ social interaction information. In [176], an adaptive transmission power control MAC protocol is proposed in order to improve the network throughput using a single channel and transceiver. By controlling the power of transmission, concurrent transmissions are enabled without interference between them. In [177], a new power-controlled MAC is proposed to increase the probability of concurrent transmissions and the durability of battery life. The survey [178] detailed the power control algorithms and classified them according to their approaches.
With the huge developments in wireless technologies and with the arrival of 5G technology, the growth of Wireless Body Area Network (WBAN) has accelerated in order to improve the human life quality. This paper aims at highlighting the most recent advances in WBAN systems as well as future challenges. The main features of WBAN systems such as power consumption, interference, latency, security, privacy, reliability and the choice of a suitable sensor, are well detailed in this paper. We also discussed the state of the art of several wireless communication technologies to determine their suitability for WBANs medical applications, including the newly emerged LPWAN communication technologies. The role to play by 5G, B5G, and 6G and their impact on the healthcare systems are also presented. Further, we point out a list of methodologies and features of a wide range of WBAN medical applications and we surveyed a wide range of sensors used in these systems regarding their size, position and their operating technique. This paper highlighted also a set of challenges and future research axes related to security and privacy of the WBAN data, adapting the emerging technologies protocols to the e-health applications, the health impact of the technologies, interference and others.
For the future perspectives of WBAN, they can be inspired from the Covid-19 pandemic. The actual situation of Covid-19 raises up several challenges related to the e-healthcare system. This pandemic proves the efficiency of WBANs in decreasing the medical cost and the contact between the patient and the medical specialists, increasing the hospitals’ capacity, and tracking the suspected cases of Covid-19. Efficient and scalable e-health systems become crucial for the future of the health care. However, the huge increase in the e-health devices raises several issues such as the network capacity and the interference management. Also, high speed data rate may be one of the main requirements for the future WBAN systems in order to carrying massive data (such as video and image data) fastly to the medical centre. With the coming of 5G and beyond, high data rate could be ensured where this technology is expected to increase the data rate 100 \(\times\) the speed of 4G. Finally, with the high spread of the WBAN systems, the data security and the patient privacy raise also high challenges. Then, efficient security techniques should be developed to protect the medical data due to its sensitivity and criticality. Furthermore, ethical laws should be considered and developed to keep the patient privacy safe.